They looked out for you
.
They looked out for you;
now you get to look out for them.
You’ve likely heard the stories . . . The widow whose family member sold her property without her knowledge and pocketed the money. The son who intercepted 7 Social Security Checks. The granddaughter who “borrowed” $30K
The FBI estimates that seniors lose more than $3 billion each year to fraudsters. And according to the National Council on Aging, over 90% of all reported elder financial abuse is committed by an older person’s own family members, most often their adult children, followed by grandchildren, nieces and nephews, and others.
Older consumers are attractive targets for financial abuse because they may have significant assets or equity in their homes and usually have a regular source of income such as Social Security or a pension. They may also be especially vulnerable due to isolation, cognitive decline, physical disability, or other health problems. In recent studies, about 17 percent of seniors reported that they have been the victim of financial exploitation, but few cases ever come to the attention of protective services.
Should you report it?
This is the most heartbreaking part: The U.S. Department of Justice states that although fraud victims are not alone, they often suffer their losses alone and in silence. Shame, guilt, embarrassment, and disbelief are among the reasons that only an estimated 15 percent of the nation’s fraud victims report their crimes to law enforcement. Other reasons include victims’ doubt about their own judgment, a sense of betrayal, and fears about how their family members, friends, and business associates will react. Some victims feel their losses are not large enough to report, do not want to get involved, think law enforcement agencies will not take the crime seriously, or think nothing will result from reporting the crime. Many victims feel they only have themselves to blame, when in reality, calculating, skilled perpetrators are to blame for these criminal acts.
Follow these three fraud safety tips:
- If you are concerned about possible fraud, remember to approach an older adult gently. They are likely ashamed or in disbelief. If someone has been a victim of fraud, act quickly so the situation doesn’t escalate.
- The Federal Trade Commission has an email service that alerts to the most current scams. AARP’s Fraud Watch Newsletter has the same purpose.
- The National Center on Elder Abuse offers specific directives on calling 911 and contacting local officials specific to your location.
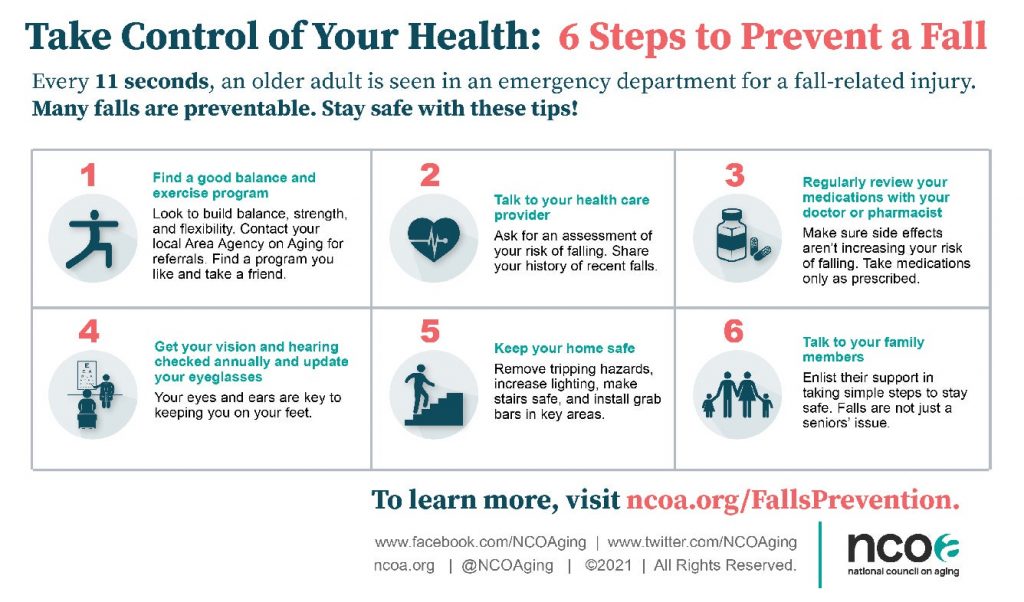
Did you know that the Ways & Wane Digital Care Advisor has an entire section dedicated to protecting the older adults in your life? Go to “I want to keep my senior safe” to find an even deeper dive into fraud protection as well as protection against falls and other safety hazards.